Abstract
Introduction: Pancreaticopleural fistula (PPF) represents a rare complication of chronic pancreatitis. The treatment is complex including pleural drainage, decompression of main pancreatic duct by endoscopic retrograde cholangiopancreatography, pancreas rest with parenteral or enteral nutrition via naso-jejunal feeding tube and somatostatin analogues application. Surgery is indicated when the conservative or endoscopic treatment is not successful. In selected cases, total pancreatectomy may be considered. After these procedures, unstable diabetes mellitus may be a problem. In this case report, the authors present an alternative way to resolve pancreatico-pleural fistula in patients with a history of pancreatic resection.
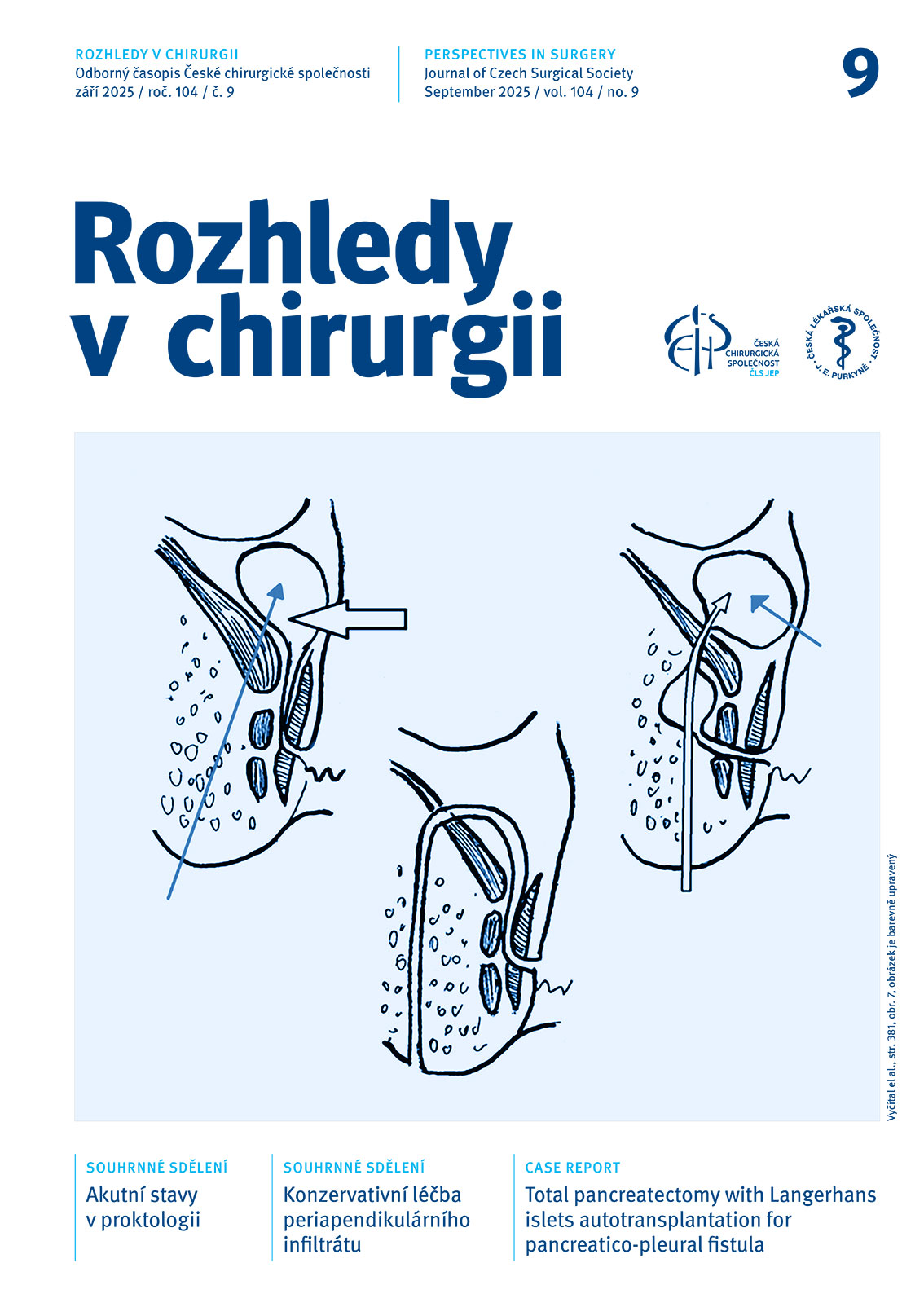
Case report: A 49-year-old man underwent pancreatoduodenectomy with pancreato-gastrostomy for chronic pancreatitis in 2018. Two years after the procedure, he had severe dyspnea, with X-ray showing left-sided fluidothorax. Pleuracentesis confirmed high amylase activity in pleural effusion. A CT scan was performed and a diagnosis of pancreaticopleural fistula was made. Due to the failure of conservative treatment, the residual pancreas was resected. The islets of Langerhans from the resected pancreatic tissue were isolated and transplanted back into the patient’s liver via the portal vein. The postoperative course was uneventful. Two year after the procedure, the patient was asymptomatic without pleural effusion recurrence and no need of insulin replacement therapy.
Conclusion: Total pancreatectomy with islet autotransplantation may be an appropriate method of treatment for recurrent pancreaticopleural fistula in situations where less radical procedures are not possible.
doi: 10.48095/ccrvch2025404